IgA1 versus IgA2 in inflammation
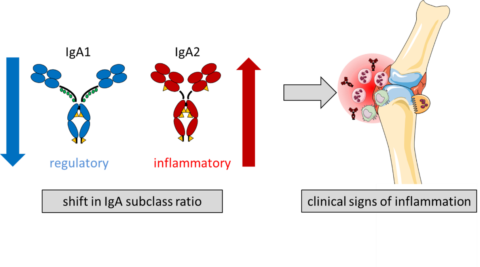
Autoantibodies directed against the body’s own structures play an important role in the development of autoimmune diseases such as rheumatoid arthritis. Antibodies occur in the form of different isotypes (IgA, IgE, IgG and IgM), which have different tasks. Previous research has mainly focused on the IgG isotype, which is the most common isotope in human blood. There is evidence that autoantibodies of the IgA isotype also contribute to the clinical picture of rheumatoid arthritis. However, the effect of IgA antibodies has so far been described ambivalently and it was unclear whether they contribute to inflammatory reactions or have an anti-inflammatory effect. A research team led by Ulrike Steffen has now discovered that the two IgA subclasses (IgA1 and IgA2) behave differently. While IgA1 does not cause inflammation and might even have a protective effect against rheumatoid arthritis, IgA2 leads to increased formation of neutrophil extracellular traps (NET) and release of inflammatory cytokines. Thus IgA2 may contribute to joint inflammation in patients with rheumatoid arthritis. The research team also found that the distribution of IgA1 and IgA2 in arthritis-specific autoantibodies is shifted in favor of pro-inflammatory IgA2 and that this shift correlates with the intensity of disease activity. They recently published their results in the magazine “Nature Communications”.
