Study in Nature unlocks how cortisone inhibits inflammation
How the body switches out of “fight” mode
Cortisone and other related glucocorticoids are extremely effective at curbing excessive immune reactions. But previously, astonishingly little was known about how they exactly do that. A team of researchers from Charité – Universitätsmedizin Berlin, Uniklinikum Erlangen and Ulm University have now explored the molecular mechanism of action in greater detail. As the researchers report in the journal Nature, glucocorticoids reprogram the metabolism of immune cells, activating the body’s natural “brakes” on inflammation. These findings lay the groundwork for development of anti-inflammatory agents with fewer and less severe side effects.
The glucocorticoid cortisone is actually naturally present in the body as cortisol, a stress hormone. The organism releases cortisol to improve the body’s responses to stress. Cortisol intervenes in sugar and fat metabolism and affects other parameters, including blood pressure and respiratory and heart rate. At higher doses, it also inhibits the activity of the immune system, which makes it useful for medical purposes: Due to their excellent efficacy, synthetic glucocorticoid derivates that inhibit inflammation, even more than the natural substance present in the body, are used to treat a wide range of immune-mediated inflammatory diseases. They are among the most widely used medications of all.
Glucocorticoids affect not only genes, but also cellular energy sources
However, glucocorticoid-based medications also have side effects, especially at higher doses and when administered for longer periods. These side effects are related to the other effects of the body’s own cortisol. They include high blood pressure, osteoporosis, diabetes, and weight gain. With the aim of developing anti-inflammatory agents with fewer and less severe side effects, a team of researchers led by Prof. Gerhard Krönke, director of the Department of Rheumatology and Clinical Immunology at Charité, has now conducted a closer study of how the immunosuppressive effects of glucocorticoids exactly works.
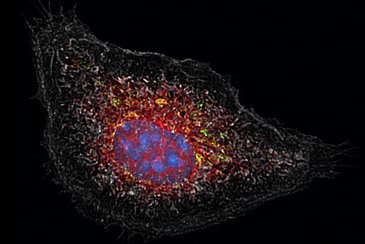
“It was previously known that glucocorticoids activate a number of genes in different cells of the body,” Krönke explains. “But through this mechanism, they mainly activate the resources present in the body. This does not adequately explains its strong immunosuppressive effect. In our study, we have now been able to show that glucocorticoids affect more than just the gene expression in immune cells. It also affects the cell´s powerhouses, the mitochondria. And that this effect on cell metabolism is in turn crucial to the anti-inflammatory effects exerted by glucocorticoids.”
Swords to plowshares
For the study, the research team focused on macrophages, a type of immune cell responsible for eliminating intruders such as viruses and bacteria. These cells can also play a role in the emergence of immune-mediated inflammatory diseases. The researchers studied how these immune cells – derived in this case from mice – responded to inflammatory stimuli in a laboratory setting and what effects additional administration of a glucocorticoid had. The researchers observed that in addition to its effect on gene expression, glucocorticoids had a major effect in reversing changes in the cell metabolism that had been initiated by the inflammatory stimuli.
“When macrophages are put into ‘fight’ mode, they redirect their cellular energy into arming for a fight. Instead of supplying energy, their mitochondria produce the components needed to fight intruders,” Krönke says, describing the processes involved. “Glucocorticoids reverse the process, switching the ‘fight’ mode back off and turning swords into plowshares, so to speak. A tiny molecule called itaconate plays an especially important role in this.”
Itaconate mediates anti-inflammatory effect of glucocorticoids
Itaconate is an anti-inflammatory substance that the body naturally produces inside its mitochondria. Macrophages produce it early on when they are activated so that the inflammatory reaction will subside after a certain period. Generation of this natural immune “brake”, however, requires sufficient fuel. When the cell´s powerhouses are arming up for a fight, that is no longer the case, so itaconate production dwindles to a halt after a while. With normal, short-term inflammation, this timing is effective because the immune response has also subsided in the meantime.
“With a persistent inflammatory stimulus, the drop-off in itaconate production is an issue because there is then no immune ‘brake’ even though the immune system is still running on all cylinders, eventually contributing to chronic inflammation,” explains Dr. Jean-Philippe Auger, a scientist at the Department of Medicine 3 – Rheumatology and Immunology at Uniklinikum Erlangen and the first author of the study. “This is where glucocorticoids intervenes. By reprogramming the mitochondrial function, they ramp up the formation of itaconate in the macrophages, restoring its anti-inflammatory effect.”
The search for new active substances
Using animal models for asthma and rheumatoid arthritis, the researchers were able to demonstrate how much the anti-inflammatory effect of glucocorticoids depends on itaconate. Glucocorticoids had no effect in animals that were unable to produce itaconate. So, if itaconate mediates the immunosuppressant effect of cortisone, wouldn’t it be possible to administer itaconate directly, instead of glucocorticoids?
“Unfortunately, itaconate isn’t a particularly good candidate as an anti-inflammatory drug, because it’s unstable, and due to its high reactivity, it could cause side effects if administered systemically,” Krönke explains. “Aside from that, we assume the processes in humans to be a bit more complex than those in mice. So our plan is to look for new synthetic compounds that are just as effective as glucocorticoids at reprogramming the mitochondrial metabolism inside immune cells, but have fewer and less severe side effects.”
About the study
The study was led by Prof. Gerhard Krönke, who initiated the work at the Department of Medicine 3 – Rheumatology and Immunology at Uniklinikum Erlangen, the medical center affiliated with Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), before moving to Charité. The first author of the publication, Dr. Jean-Philippe Auger, still works there. Jan Tuckermann, Professor at Ulm University and Dr. Eicke Latz, Professor of Experimental Rheumatology at Charité and Scientific Director of the German Rheumatism Research Centre Berlin (DRFZ), a Leibniz Institute, also contributed to the study. Krönke and Latz are working together in Berlin to develop new anti-inflammatory drugs and advance personalization in the field of rheumatology.
Further information:
Sandra Jeleazcov
Department of Medicine 3
+ 49 9131 85 39109
sandra.jeleazcov@uk-erlangen.de
